Ovarian cancer survival linked to protein
Date 20.09.2017
20.09.2017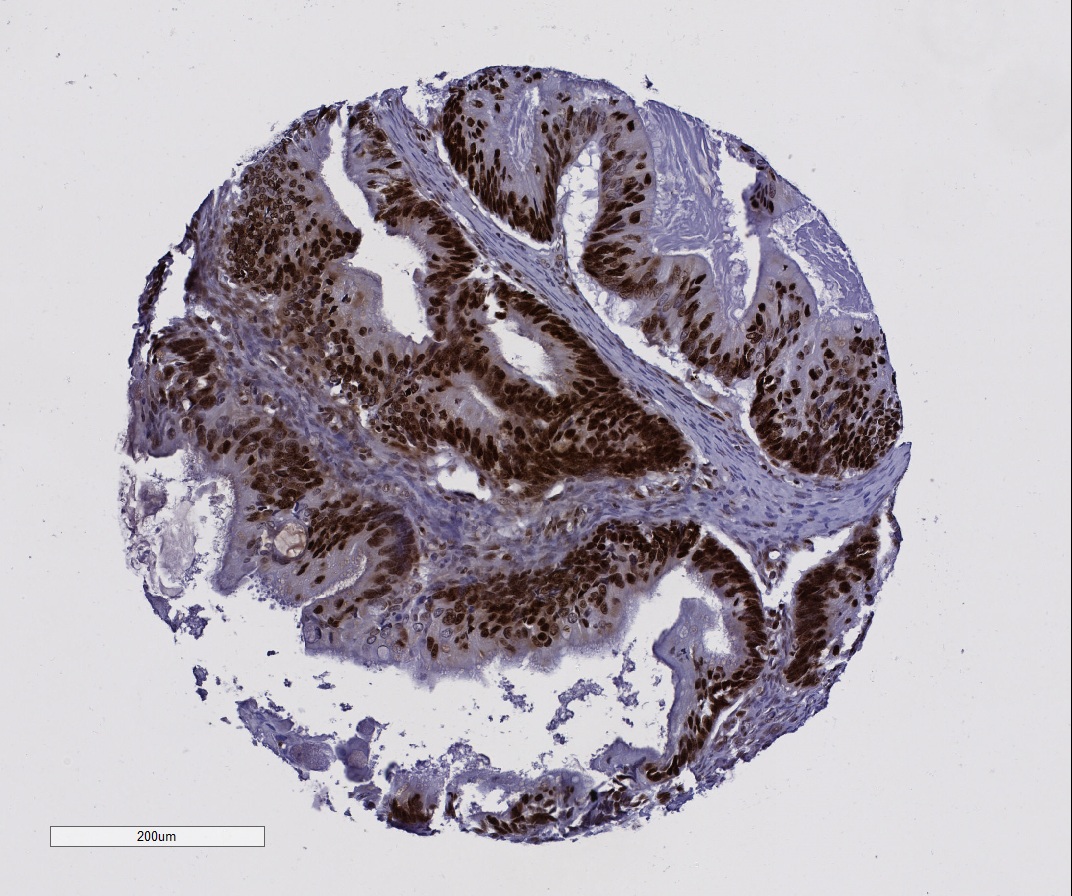
The chances of surviving ovarian cancer may be drastically affected by the production of a specific protein, according to new research led by the University of Northampton.
In a study of more than 500 cases, patients with no, or very low, amounts of the DNA binding protein survived twice as long than those whose tumours produced much greater levels.
The results have important implications for diagnosing and treating the disease.
Lead author Dr Lee Machado, Associate Professor in Biochemistry, said the high-mobility group protein B1 (HMGB1) should now be considered as a target for new treatments.
“High levels of HMGB1 are also known to confer tumours with resistance to therapy, and future studies should determine the exact mechanism of HMGB1 function in ovarian cancer.
“If this can be determined, then strategies designed to disrupt HMGB1 production may one day produce new therapies.”
The findings, published in the journal Oncotarget, show that expression of HMGB1 was associated with reduced average survival time from almost nine years in patients with low or absent expressing tumours, to just over four and a half years for those with high expressing tumours.
Eleven women die from the disease every day in the UK – the sixteenth highest such figure in Europe.
It is still unclear the mechanism by which this protein impacts survival, but HMGB1 may play a role in increasing the amount of energy produced by tumour cells.
“This energy is then used by cancer cells to grow, multiply, and ultimately spread throughout the body,” said Dr Machado, who conducted the research with colleagues from the University of Nottingham.
The team looked at tissue samples from 194 cases of epithelial ovarian cancer treated at Nottingham University Hospitals, and 360 cases that had been treated at Derby City Hospitals.
High levels of the protein were associated with poor progression free survival in the Nottingham cases and poor overall survival in the Derby ones.
In the UK, over 7,000 women a year develop the disease, with epithelial ovarian cancer the most common type. Just over half of diagnoses are in women over the age of 65.
Chances of surviving the disease for longer than five years drop dramatically from around ninety percent to less than twenty, when comparing women with early and late stage diagnoses.
Referring to the potential of using HMGB1 as a diagnostic tool, Dr Machado said: “It could really improve both our understanding of ovarian cancer biology, and treatment of these patients.”
The HMGB1 protein has so far been implicated in a range of cancers including bowel, lung and liver and recent studies have focused on its ability to protect cancer cells from stresses – such as chemotherapy – through a process known as autophagy.
Machado, L., Moseley, P. M., Moss, R., Deen, S., Nolan, C., Spendlove, I. and Ramage, J. (2017) High mobility group protein B1 is a predictor of poor survival in ovarian cancer. Oncotarget 1949-2553.
Ovarian Cancer Statistics
(data courtesy of Cancer Research UK )
There were around 7,400 new cases of ovarian cancer in the UK in 2014.
In females in the UK, ovarian cancer is the fifth most common cause of cancer death, with around 4,100 deaths in 2014.
In Europe, around 42,700 women were estimated to have died from ovarian cancer in 2012. The UK mortality rate is 16th highest in Europe.
More than half (53%) of ovarian cancer cases in the UK each year are diagnosed in females aged 65 and over (2012-2014).
There are no UK-wide statistics available for ovarian cancer survival by stage. Survival statistics are available for each stage of ovarian cancer in one area of England. These are for women diagnosed between 2002 and 2006.
In (early) Stage 1, about 90 percent will survive their cancer for five years or more after they are diagnosed. For Stage 2 it is more than 40 percent; Stage 3 almost 20 percent; and in (late) Stage 4, around five percent.