BLOG: Delight and controversy over new drug to treat Duchenne muscular dystrophy
Date 23.09.2016
23.09.2016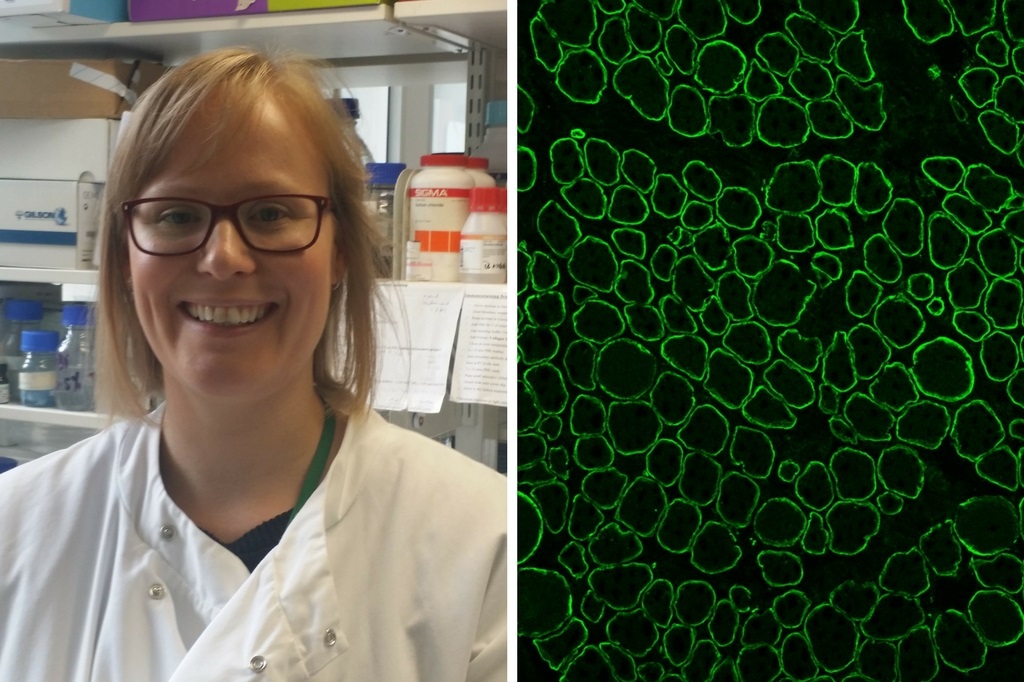
Dr Karen Anthony, lecturer in molecular bioscience at the University of Northampton, explains the controversy behind a new drug to treat Duchenne muscular dystrophy.
“This week, a drug to treat Duchenne muscular dystrophy (DMD) was granted accelerated approval by the United States Food and Drug Administration (FDA). The long awaited decision on a drug that may improve the lives of those suffering with Duchenne is of course welcome news, but its approval has been highly controversial. The FDA have ruled that, in this case, the consequences of not approving an effective drug would be far greater than approving an ineffective drug.
DMD is a rare, 100% fatal, childhood genetic disorder that overwhelmingly affects boys. It is characterised by muscle weakness and breakdown leading to death in early adulthood. The drug, branded Exondys 51 (generic name: eteplirsen) forms a ‘molecular patch’ over the causative DNA mutations of approximately 13% of boys with Duchenne. That’s right. It can only treat 13% of individuals with DMD who harbour the most common mutations. Other drugs of the same type are currently in development to treat boys with different mutations. It is hoped that approval of the first ‘Exondys’ drug can smooth the pathway for other such drugs.
The accelerated approval program was designed to allow faster approval of drugs for rare, serious, conditions that meet an unmet medical need. Based on initial data, Exondys 51 will now be available to applicable patients in America but Sarepta Therapeutics, the company that made the drug, is required to perform a confirmatory clinical trial to prove that the drug does indeed offer a meaningful clinical benefit to patients. The FDA may withdraw approval if this cannot be demonstrated.
So why is this controversial? Exondys 51 is designed to kickstart the production of a protein called dystrophin. Dystrophin is missing from the muscles in patients with DMD, and its absence is responsible for the severe muscular symptoms. Sarepta have indeed demonstrated that Exondys 51 treatment can increase the levels of dystrophin. However, the observed increase is small and we do not yet know how much dystrophin is needed to functionally improve the lives of those with Duchenne. Critics argue that Sarepta failed to provide sufficiently adequate data for even the accelerated approval pathway and that the observed levels of dystrophin are not likely to provide a meaningful clinical benefit. Beyond that, the design of the clinical trial and the method used to measure dystrophin have been heavily criticised.
The eventual decision to approve Exondys 51 overrules an advisory panel who voted 7-3 (with three abstentions) against approval. Approval launched an unprecedented scientific dispute within the FDA itself and accusations that the director of the Centre for Drug Evaluation and Research bowed down to pressures from advocacy groups. The lobbying of patient and parent groups at every stage of clinical development has been incredible and likened to that observed during the AIDS crisis of the 1980’s. Approval must always be based on science, one lesson we can take from this experience is that an early constructive dialogue between all stakeholders can accelerate the development of new treatments for rare orphan diseases.
I have seen evidence of Exondys 51 efficacy with my own eyes down the microscope working as part of the team that originally developed the drug in the UK. I am absolutely delighted our early work has contributed to a treatment option for boys with Duchenne muscular dystrophy. I only hope Exondys 51 can make a return journey across the pond and improve the symptoms of those boys who took part in the first clinical trials here in the UK.”
For more information regarding Dr Anthony’s research, visit her ResearchGate page.